Pregnancy is often talked about as though it's a light switch. You're a regular person walking around and then a switch flips — presto, you're pregnant.
The reality is more nuanced.
"Sex ed really oversimplified it: 'The egg has been fertilized and it has implanted,'" says Carmel Shachar, who runs the Petrie-Flom Center for Health Law Policy, Biotechnology, and Bioethics at Harvard Law School. "What people don't realize is that there's a whole, very complex journey before that, that honestly usually is invisible."
Lots of steps need to happen, she says, from the time an egg and sperm meet to the moment a person tests positive on a pregnancy test.
The more scientists learn, the more they realize that the start of pregnancy isn't a moment, but a process that often ends before it really begins. As many as 1 in 3 fertilized eggs either won't implant or will end in miscarriage. In fact, most pregnancy loss happens before the fertilized egg implants.
Defining exactly when a pregnancy begins is a hot topic in some state legislatures and U.S. courts at the moment. While federal law has long said pregnancy starts after a fertilized egg has implanted in the uterus, state law in Kentucky, for example, calls someone pregnant as soon as a sperm meets the egg.
With so much riding on biology that's often misunderstood, let's break down what is known: Here's how the run-up to a pregnancy begins in that very first week of action, from the minute a single egg, the size of a grain of table salt, bursts forth from an ovary.
DAY 0
Ovulation

Starting at puberty, a process called ovulation begins. That's when — roughly once a month — a single mature egg breaks through its surrounding capsule, or follicle, and is released from one of the ovaries.

If you were born with ovaries, you were born with all the eggs you'll ever have — roughly 1 million to 2 million. Each month, about 1,000 eggs are activated but never develop further, while one (or sometimes a couple) fully matures. This happens until menopause, usually several decades later, when there aren't many eggs left.

After it's released from the follicle, the egg is scooped up and enveloped by the nearby, fingerlike projections (also known as fimbriae) at the end of one of the two slender uterine tubes (sometimes called fallopian tubes) that lead to the uterus.
The egg is protected by two layers. The inner one is called the zona pellucida, a jelly cushion of protein. The outer layer is called the corona radiata — a sunlike array of helper cells that have been nurturing the egg inside the ovary. These protective layers become even more important later.
Anatomy of the human egg

(Assisted reproductive technologies have greatly expanded how ovulation and fertilization can happen so that many more people can have babies. What we're describing here is what happens when that assistance isn't needed.)
The uterine tube acts as a kind of pulsing walkway; it's lined with cilia (small hairlike structures) that beat rhythmically, moving the egg along. Once the egg leaves the ovary, there's only a short window — less than 24 hours — for fertilization to happen.
Meanwhile, a lot has been happening in the uterus. For weeks, rising levels of the hormone estrogen have prompted a thickening of the endometrium — that's the cushiony lining of the uterus. The endometrium is one of the fastest-growing tissues in the body — in a monthlong menstrual cycle, it can grow to eight times its initial thickness.
The 28-day cycle of the endometrium

If sexual intercourse happens the same day as ovulation (or even several days beforehand), that's when sperm may enter the picture.
Every ejaculation contains tens of millions of sperm, and sperm can survive up to five days or so inside the uterus or uterine tubes.
Anatomy of a sperm

Now, despite what you may have heard, sperm cells are not a mighty infantry on a self-propelled mission to get to the passive egg.
Those little tails do give sperm some mobility by moving in a corkscrew motion, but sperm don't have enough energy or directional ability to get to an egg on their own.

In fact, most sperm don't get very far. Crossing the uterus to get to the egg in whichever uterine tube it is in means navigating an immense distance with lots of crevices to get lost in and immune cells to evade.
Scientists think waves of fluid inside the uterus, body heat, chemical signals, beating cilia and muscular contractions of the uterus (possibly from sex) play a role in how quickly sperm get to one of the uterine tubes. Some can get there within an hour of intercourse!
Only a small percentage of the sperm make it that far.
DAY 1
Fertilization

Once inside the uterine tube, the sperm become hyperactivated (for reasons researchers still don't understand) and begin to move more vigorously.

When they reach the egg, the sperm still aren't done. There are those two layers that encapsulate the egg — the corona radiata and the jellylike zona pellucida — to get through before fertilization can happen.

Enzymes released by the sperm help break down these layers. When the first sperm gets through the corona radiata, through the zona pellucida and, finally, through the membrane of the egg itself, the egg releases enzymes that quickly harden the zona. No other sperm can get in at this point. The first sperm that reaches the egg and attaches to its outer membrane releases its genetic material into the egg.
This is the moment of fertilization, otherwise known as conception. It has been less than a day since the egg was released from the ovary, and there are still many uncertainties to overcome before this fertilized egg becomes an embryo.

The egg and sperm each have 23 chromosomes (most other cells in the body have 46 — in 23 pairs). Through the process of fertilization, the 23 chromosomes from the egg and the 23 from the sperm join together and mix a bit to create a new, unique genetic blueprint.
The egg, now fertilized and containing its new set of 23 pairs of chromosomes, is called a zygote. The genes that will influence hundreds of characteristics — ranging from biological sex to hair color and eye color — are determined instantly.
DAY 2
Division

Very quickly, the one-celled zygote starts to divide and travel again through the uterine tube. One cell becomes two, then four, then eight, then 16. The cells of the corona radiata that had been surrounding the egg start to fall off, disperse and eventually disappear.

DAYS 3 and 4
Travel time

The eight-to-32-cell stage looks kind of like a berry, so the bundle is called a morula, which is Latin for mulberry.
Even as the morula continues to divide into dozens of cells and then hundreds, its outer case, the now-hardened zona, keeps it from expanding in size — so it's still only about as big as a grain of salt. That's crucial to keep the little ball of cells from getting stuck as it moves through the slender uterine tube.
DAY 5
Entering the uterus

Four days after fertilization, the fertilized egg has become a blastocyst — a bundle of cells with certain structures. Some will become the placenta, and others the embryo.

The blastocyst has now traveled all the way down the uterine tube. Around this time, the bundle of cells breaks out of its zona covering so it's able to implant in the lining of the uterus — the endometrium.

Now inside the uterus, a week or so after ovulation, the blastocyst has about four days to implant in the soft-tissue lining of the uterus.
DAY 6
Implantation begins

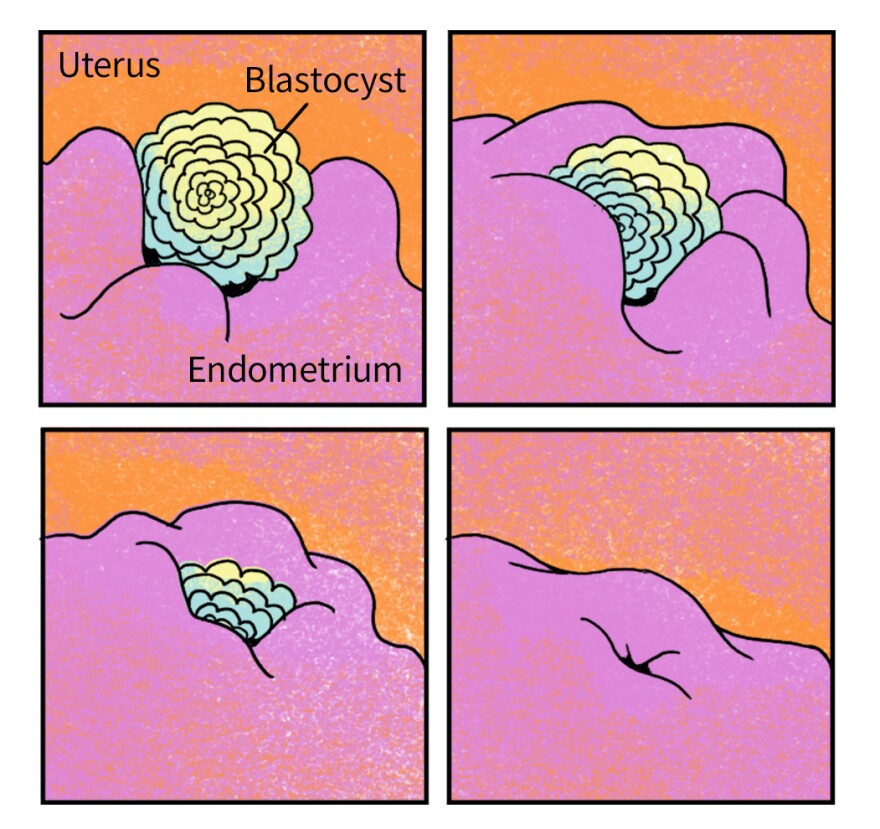
Voilà — this is implantation, considered the start of pregnancy under U.S. federal law.

At this point — about a week after ovulation — the person who has had all these changes happening inside their body still has no idea it has been going on. It will take an additional week after implantation (at the earliest) before there's enough of a hormone called hCG in their urine to turn a home pregnancy test positive. That's right around the time some people with very regular cycles might notice that their period is late.

For all the fascinating things scientists know about how all this happens, there's still so much that's not yet well understood. Early pregnancy remains something of a black box. At the moment, there's limited technology to be able to observe — let alone intervene — in very early pregnancy, which is why so many of the details are still unknown. "It's happening inside a person, and it's very difficult to study without disturbing the pregnancy," notes Shachar, the Harvard bioethicist.
That's a challenge for laws that try to regulate pregnancy, Shachar says. "The take-away is that a lot of legislation in this area doesn't reflect scientific knowledge, especially because laws don't work well with scientific uncertainty."

As science and politics continue to clash over when life begins, understanding the process of early pregnancy as fully as possible is more important than ever.
We created a printable version of this guide. Download and print it here.
Thanks to the many scientists who offered guidance and advice for this story, including Ripla Arora of Michigan State University, David Miller of the University of Illinois Urbana-Champaign and Joanne Muter of the University of Warwick, among others.
Illustrations by LA Johnson; edited by Meredith Rizzo and Deborah Franklin; visual design by LA Johnson, Meredith Rizzo, Alyson Hurt; researched and fact-checked by Will Chase; copyedited by Preeti Aroon.
Copyright 2023 NPR. To see more, visit https://www.npr.org.








