A year ago, John Nute couldn’t brush his teeth with his left arm, drive with both hands or peel shrimp. A stroke in 2013 had immobilized much the left side of his body. He’d lost the job he loved running a marina and the housing that came with it.
But Nute’s life changed significantly over the last 12 months following the implant of a technology known as Vivistim that’s gaining attention in Connecticut.
State lawmakers are looking to establish a program at the University of Connecticut, where 10 veterans will be able to undergo the procedure for free and physicians will conduct further research to improve the effectiveness of the treatment. The $55.7 billion two-year budget adopted by the legislature’s Appropriations Committee on Tuesday includes $2 million in fiscal year 2027 to establish a Center of Excellence for Neuromodulation Treatment at UConn.
The Vivistim device, implanted in a patient’s neck and chest, includes a battery and a narrow cable that wraps around the vagus nerve. When turned on, the device sends electrical signals to the brain.
Neuromodulation, as it’s known, refers to the process of altering how the brain receives information from the body by stimulating nerves.
For reasons physicians still don’t entirely understand, employing neuromodulation by stimulating the vagus nerve through electric signals appears to rapidly increase the rate at which the brain learns new tasks. When paired with physical therapy, the device can help stroke survivors regain lost functionality — even if, like Nute, their stroke occurred several years earlier.
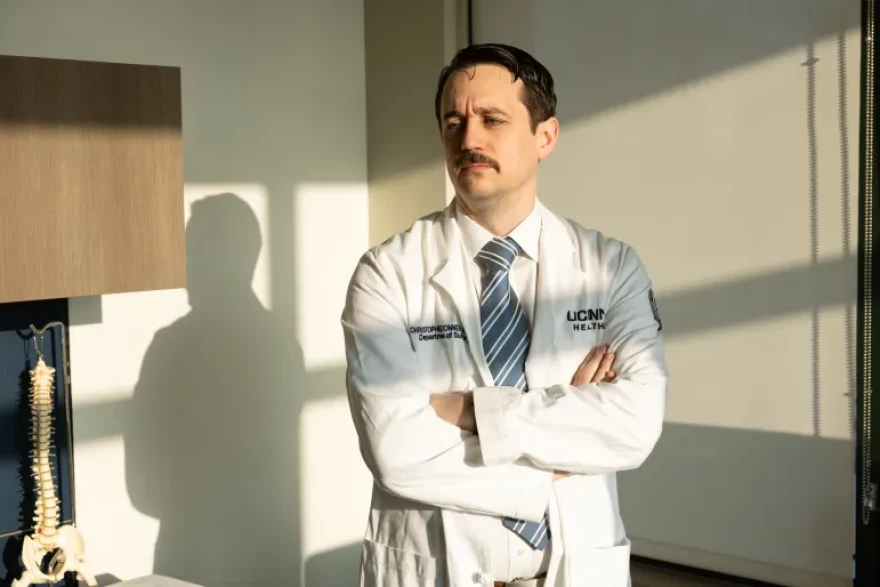
“It supercharges therapy,” Christopher Conner, the UConn neurosurgeon who performed the procedure on Nute. “You basically get into a state where your brain is able to learn or adapt more quickly,” he said.
Conner was among a group of physicians on the state’s Veterans with Disabilities Task Force who sought funding from the legislature to cover the procedure at UConn and subsequent rehabilitation at Hartford HealthCare for ten veterans. The funding would offer much-needed health care to an underserved group, as well as provide physicians and researchers with more data about how exactly the procedure improves results for stroke patients, according to supporters.

How does it work?
People who suffer strokes often hit a recovery plateau beyond which it’s difficult for them to continue making progress towards regaining mobility.
Neuromodulation offers results far beyond what’s been available in stroke recovery up to this point, according to several providers in the state. Connecticut physicians said they’ve seen patients regain basic functionality and return to hobbies — like cooking, playing guitar, and golfing — that they had to give up after their stroke.
Nute was still struggling with physical side effects when he saw an advertisement on Facebook promoting a new technology that could boost hand and arm function after a stroke.
“I just got tired of having my mobility impaired and wanted to improve it,” Nute said. Eager for results and open to new solutions, Nute reached out to the company and then an occupational therapist to learn more.
When they met roughly a month later, in January 2024, Conner told Nute that he wanted to be transparent: He had never done the procedure before.
“I said, ‘Well, I haven’t either, so that’s two of us,’” Nute recalled with a laugh.
Nute underwent the procedure in May of 2024, and since then he said his range of motion has increased significantly. He loves to cook, so he’s most excited about the accomplishments that translate to the kitchen. Nute still attends group rehabilitation regularly, both in-person and on Zoom, and he also receives Botox injections every three months that help to relax the muscles in his arm.
“When I first got the thing done, I wasn’t noticing improvements right away,” Nute said. But over time, he said, that changed. “When I look at videos of myself before and after, I can see significant differences.”

Conner has now done a total of 12 implants, with another five booked in the next few months. He said he gets calls weekly from patients all over the country who want to come to Connecticut for the procedure.
“The interest in this is unbelievable,” Conner said during public testimony at the state legislature. “Here at the University of Connecticut, we’ve established ourselves as a nation-leading center for this.”
Vagus nerve stimulation isn’t entirely new, Conner said. It’s been used in the past to treat seizures and depression, with limited results. But using the treatment for stroke recovery is novel — the Food and Drug Administration approved Vivistim to treat upper extremity impairments post-stroke in August 2021.
The real “magic,” as Conner puts it, happens in therapy, which patients begin two weeks after getting the implant. For six weeks, patients attend rehabilitation three times a week, for 90 minutes per session. The sessions focus on completing upper extremity exercises, like reach and grasp, object flipping and needle threading.

Each task is repeated about 50 times, and patients might perform a total of 300 repetitions in a single session, Subramani Seetharama, a rehabilitation specialist at Hartford HealthCare, said. As the patient performs these exercises, the physician turns on the Vivistim system, which sends those electric signals to the patient’s brain.
Seetharama, who’s been practicing medicine for 30 years, said he’s been frustrated that treatments available to stroke patients up until now have only offered temporary improvements.
“It’s been kind of disappointing,” Seetharama said. “But here I see an amazing, lasting, persistent improvement in strength and function.”
Carolyn Brown, cofounder of StrokeOT Inc. and an occupational therapist who has treated Nute and other Vivistim patients, stated in written public hearing testimony that she has “witnessed truly miraculous results.”
“Vivistim has given chronic stroke survivors renewed hope and optimism for their continued recovery journey,” she wrote.

State funding
Physicians still have lots of questions about how the mechanics of neuromodulation helps facilitate better results for stroke patients.
The proposed state funding would go towards studying brain activity in patients at different points in their treatment. It would also fund research on the effects of the treatment on patients’ ability to walk. Vivistim is currently only FDA-approved for upper extremity recovery.
“One of the dirty secrets of many things in modern medicine is we have a poor understanding of how it works,” Conner said. “The problem with that is that it makes it very difficult to make to optimize that therapy. So what we want to do is we want to figure out what parts of the brain are actually leading to this improved learning ability.”
Richard Foust, CEO of Vivistim distributor MicroTransponder Inc., said in emailed comments that “the company applauds UConn Health, Hartford HealthCare and all the champions of this bill for bringing it closer to fruition.”
“MicroTransponder is incredibly honored that this legislation will make Vivistim available to our Veterans to improve their hand and arm function post-stroke,” wrote Foust.
During the public hearing for the proposal, Rep. Tracy Marra, R-Darien, asked whether there are other potential funding sources for this treatment and research outside of the state government. Conner said that in the current environment, much of grant funding is on hold.
“Granting agencies and the program officers are telling people that nothing is getting reviewed,” Conner said.

Nute said the idea of more people getting access to Vivistim is “wonderful” and that funding for research is “needed.” More than a decade after his stroke, he remains deeply involved in the survivor community. He serves on the board of a stroke survivors support group and regularly speaks about his experience with neuromodulation.
“I talk to people virtually everyday who’ve either had a stroke or they know somebody that’s had a stroke and try to get them thinking that this is not the end of the road,” Nute said. “There is hope. Don’t give up.”




